Summary: Researchers have designed a new method of converting non-neural cells into functioning neurons that are able to form synapses, dispense dopamine, and restore the function of neurons undermined by Parkinson’s associated destruction of dopaminergic cells.
Source: Arizona State University
Neurodegenerative diseases damage and destroy neurons, ravaging both mental and physical health. Parkinson’s disease, which affects over 10 million people worldwide, is no exception. The most obvious symptoms of Parkinson’s disease arise after the illness damages a specific class of neuron located in the midbrain. The effect is to rob the brain of dopamine—a key neurotransmitter produced by the affected neurons.
In new research, Jeffrey Kordower and his colleagues describe a process for converting non-neuronal cells into functioning neurons able to take up residence in the brain, send out their fibrous branches across neural tissue, form synapses, dispense dopamine and restore capacities undermined by Parkinson’s destruction of dopaminergic cells.
The current proof-of-concept study reveals that one group of experimentally engineered cells performs optimally in terms of survival, growth, neural connectivity, and dopamine production, when implanted in the brains of rats.
The study demonstrates that the result of such neural grafts is to effectively reverse motor symptoms due to Parkinson’s disease.
Stem cell replacement therapy represents a radical new strategy for the treatment of Parkinson’s and other neurodegenerative diseases. The futuristic approach will soon be put to the test in the first of its kind clinical trial, in a specific population of Parkinson’s disease sufferers, bearing a mutation in the parkin gene.
The trial will be conducted at various locations, including the Barrow Neurological Institute in Phoenix, with Kordower as principal investigator.
“We cannot be more excited by the opportunity to help individuals who suffer from this genetic form of Parkinson’s disease, but the lessons learned from this trial will also directly impact patients who suffer from sporadic, or non-genetic forms of this disease,” Kordower says.
Kordower directs the ASU-Banner Neurodegenerative Disease Research Center at Arizona State University and is the Charlene and J. Orin Edson Distinguished Director at the Biodesign Institute. The new study describes in detail the experimental preparation of stem cells suitable for implantation to reverse the effects of Parkinson’s disease.
The research appears in the current issue of the journal Nature Regenerative Medicine.
New perspectives on Parkinson’s disease
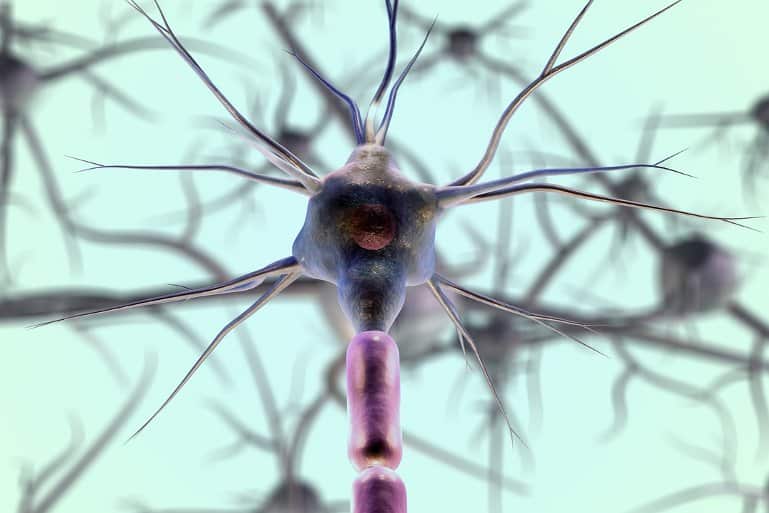
You don’t have to be a neuroscientist to identify a neuron. Such cells, with their branching arbor of axons and dendrites are instantly recognizable and look like no other cell type in the body. Through their electrical impulses, they exert meticulous control over everything from heart rate to speech. Neurons are also the repository of our hopes and anxieties, the source of our individual identity.
Degeneration and loss of dopaminergic neurons causes the physical symptoms of rigidity, tremor, and postural instability, which characterize Parkinson’s disease. Additional effects of Parkinson’s disease can include depression, anxiety, memory deficit, hallucinations and dementia.
Due to an aging population, humanity is facing a mounting crisis of Parkinson’s disease cases, with numbers expected to swell to more than 14 million globally by 2040. Current therapies, which include use of the drug L-DOPA, are only able to address some of the motor symptoms of the disease and may produce serious, often intolerable side effects after 5-10 years of use.
There is no existing treatment capable of reversing Parkinson’s disease or halting its pitiless advance. Far-sighted innovations to address this pending emergency are desperately needed.
A (pluri) potent weapon against Parkinson’s
Despite the intuitive appeal of simply replacing dead or damaged cells to treat neurodegenerative disease, the challenges for successfully implanting viable neurons to restore function are formidable. Many technical hurdles had to be overcome before researchers, including Kordower, could begin achieving positive results, using a class of cells known as stem cells.
The interest in stem cells as an attractive therapy for a range of diseases rapidly gained momentum after 2012, when John B. Gurdon and Shinya Yamanaka shared the Nobel Prize for their breakthrough in stem cell research.
They showed that mature cells can be reprogrammed, making them “pluripotent”—or capable of differentiating into any cell type in the body.
These pluripotent stem cells are functionally equivalent to fetal stem cells, which flourish during embryonic development, migrating to their place of residence and developing into heart, nerve, lung, and other cell types, in one of the most remarkable transformations in nature.
neural alchemy
Adult stem cells come in two varieties. One type can be found in fully developed tissues like bone marrow, liver, and skin. These stem cells are few in number and generally develop into the type of cells belonging to the tissue they are derived from.
The second kind of adult stem cells (and the focus of this study) are known as induced pluripotent stem cells (iPSCs). The technique for producing the iPSCs used in the study occurs in two phases. In a way, the cells are induced to time travel, initially, in a backward and then a forward direction.
First, adult blood cells are treated with specific reprogramming factors that cause them to revert to embryonic stem cells. The second phase treats these embryonic stem cells with additional factors, causing them to differentiate into the desired target cells—dopamine-producing neurons.

“The major finding in the present paper is that the timing in which you give the second set of factors is critical,” Kordower says. “If you treat and culture them for 17 days, and then stop their divisions and differentiate them, that works best.”
pitch perfect neurons
The study’s experiments included iPSCs cultured for 24 and 37 days, but those cultured for 17 days prior to their differentiation into dopaminergic neurons were markedly superior, capable of surviving in greater numbers and sending out their branches over long distances.
“That’s important,” Kordower says, “because they’re going to have to grow long distances in the larger human brain and we now know that these cells are capable of doing that.”
Rats treated with the 17-day iPSCs showed remarkable recovery from the motor symptoms of Parkinson’s disease. The study further demonstrates that this effect is dose dependent.
When a small number of iPSCs were grafted into the animal brain, recovery was negligible, but a large complement of cells produced more profuse neural branching, and complete reversal of Parkinson’s symptoms.
See also

The initial clinical trial will apply iPSC therapy to a group of Parkinson’s patients bearing a particular genetic mutation, known as a Parkin mutation. Such patients suffer from the typical symptoms of motor dysfunction found in general or idiopathic Parkinson’s, but do not suffer from cognitive decline or dementia.
This cohort of patients provides an ideal testing ground for cell replacement therapy. If the treatment is effective, larger trials will follow, applying the strategy to the version of Parkinson’s affecting most patients stricken with the disease.
Further, the treatment could potentially be combined with existing therapies to treat Parkinson’s disease. Once the brain has been seeded with dopamine-producing replacement cells, lower doses of drugs like L-DOPA could be used, mitigating side effects, and enhancing beneficial results.
The research sets the stage for the replacement of damaged or dead neurons with fresh cells for a broad range of devastating diseases.
“Patients with Huntington’s disease or multiple system atrophy or even Alzheimer’s disease could be treated in this way for specific aspects of the disease process,” Kordower says.
About this Parkinson’s disease research news
Author: press office
Source: Arizona State University
Contact: Press Office – Arizona State University
Image: The image is in the public domain
Original Research: Open access.
“Optimizing maturity and dose of iPSC-derived dopamine progenitor cell therapy for Parkinson’s disease” by Benjamin M. Hiller et al. Nature Regenerative Medicine
Abstract
Optimizing maturity and dose of iPSC-derived dopamine progenitor cell therapy for Parkinson’s disease
In pursuit of treating Parkinson’s disease with cell replacement therapy, differentiated induced pluripotent stem cells (iPSC) are an ideal source of midbrain dopaminergic (mDA) cells. We previously established a protocol for differentiating iPSC-derived post-mitotic mDA neurons capable of reversing 6-hydroxydopamine-induced hemiparkinsonism in rats.
In the present study, we transitioned the iPSC starting material and defined an adapted differentiation protocol for further translation into a clinical cell transplantation therapy.
We examined the effects of cellular maturity on survival and efficacy of the transplants by engrafting mDA progenitors (cryopreserved at 17 days of differentiation, D17), immature neurons (D24), and post-mitotic neurons (D37) into immunocompromised hemiparkinsonian rats.
We found that D17 progenitors were markedly superior to immature D24 or mature D37 neurons in terms of survival, fiber outgrowth and effects on motor deficits. Intranigral engraftment to the ventral midbrain demonstrated that D17 cells had a greater capacity than D24 cells to innervate over long distance to forebrain structures, including the striatum.
When D17 cells were assessed across a wide dose range (7,500-450,000 injected cells per striatum), there was a clear dose response with regards to numbers of surviving neurons, innervation, and functional recovery. Importantly, although these grafts were derived from iPSCs, we did not observe teratoma formation or significant outgrowth of other cells in any animal.
These data support the concept that human iPSC-derived D17 mDA progenitors are suitable for clinical development with the aim of transplantation trials in patients with Parkinson’s disease.